Featured Articles
- Exploring the Untapped Potential of Gaming Communities in Cancer Support and Awareness
- Harnessing Sound Waves: Exploring Sonic Therapies as an Untapped Aid in Cancer Recovery Programs
- Rediscovering Nature: The Unexplored Healing Power of Indigenous Plants in Cancer Therapy
- The Hidden Role of AI: How Technology is Shaping Cancer Support Networks and Resources
- Top 7 Breakthrough Cancer Care Products Launched in the Last 5 Years: In-Depth Reviews & Rankings
Top 7 Breakthrough Cancer Care Products Launched in the Last 5 Years: In-Depth Reviews & Rankings
Top 7 Breakthrough Cancer Care Products Launched in the Last 5 Years: In-Depth Reviews & Rankings
Top 7 Breakthrough Cancer Care Products Launched in the Last 5 Years: In-Depth Reviews & Rankings
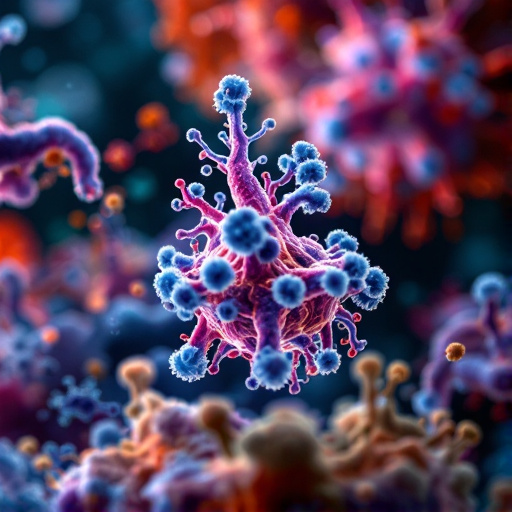
The landscape of cancer care has witnessed remarkable innovation over the past five years, introducing groundbreaking therapies and technologies that are transforming patient outcomes. From novel immunotherapies to advanced diagnostic tools, these products are redefining standards of care globally. This article provides an in-depth review and ranking of the top seven breakthrough cancer care products launched recently, highlighting their clinical impact, technological advancement, and patient benefits.
Each section of this article will focus on one key product, elaborating on its mechanism of action, clinical trial results, and real-world applications. We aim to provide healthcare professionals, patients, and caregivers with clear, evidence-based information on these innovations. Insights are based on published clinical data, regulatory approvals, and expert analyses to ensure a comprehensive understanding of each product's contribution to cancer treatment.
By exploring these cutting-edge cancer care products, the article sheds light on how recent advances are paving the way toward more personalized, effective, and less invasive cancer therapies. From early detection to targeted therapy, these innovations offer new hope for better survival rates and quality of life among cancer patients worldwide.
1. CAR-T Cell Therapy: Breyanzi (Lisocabtagene Maraleucel)
Breyanzi, approved by the FDA in 2021, is a next-generation CAR-T cell therapy designed to treat certain types of large B-cell lymphoma. This personalized treatment involves engineering a patient’s T-cells to target and destroy cancer cells expressing the CD19 antigen. Unlike earlier CAR-T therapies, Breyanzi offers a defined composition of T-cell subsets, which is associated with improved safety and efficacy.
Clinical trials highlighted its ability to induce durable remissions in patients with refractory or relapsed lymphoma. The TRANSCEND NHL 001 study demonstrated an overall response rate (ORR) of over 70%, with manageable adverse effects, primarily cytokine release syndrome and neurotoxicity. Its ability to provide long-term remission signals a significant advancement in hematologic cancer therapeutics (Locke et al., 2021, NEJM).
Breyanzi's introduction expands the options available for hematologic malignancies and represents a considerable leap forward in precision immuno-oncology. Its tailored approach and encouraging clinical outcomes underscore the growing potential of CAR-T technology in cancer care.
2. Tumor-Treating Fields (TTFields): Optune Lua
Optune Lua is a wearable device delivering Tumor-Treating Fields (TTFields) to disrupt cancer cell division using low-intensity, alternating electric fields. Approved for glioblastoma multiforme (GBM) in 2019, Optune Lua offers a non-invasive, adjunct therapy to standard chemotherapy, with minimal systemic side effects.
The EF-14 phase 3 trial demonstrated an improvement in median overall survival from 16 months to approximately 20.9 months when TTFields were combined with temozolomide chemotherapy. The device’s ability to interfere with mitotic spindle formation represents a novel anti-cancer mechanism independent of traditional cytotoxic agents (Stupp et al., 2017, JAMA).
Optune Lua’s user-friendly design promotes compliance and quality of life, marking a significant therapeutic advancement for a tumor type with historically poor prognosis. Its innovative mechanism expands the arsenal against solid tumors where conventional therapies often fall short.
3. KRAS G12C Inhibitors: Lumakras (Sotorasib)
Lumakras, approved in 2021, is the first targeted inhibitor for KRAS G12C-mutated non-small cell lung cancer (NSCLC). KRAS mutations were long deemed “undruggable,” making this advancement a landmark in oncogenic pathway targeting. Lumakras selectively binds to the mutant KRAS G12C protein, locking it in an inactive state to block tumor growth signaling.
The CodeBreaK 100 trial showed an ORR of 36% in heavily pre-treated NSCLC patients, with a median duration of response lasting nearly 11 months. Its oral administration and specificity for KRAS mutations offer a precision medicine approach with a favorable toxicity profile (Skoulidis et al., 2021, NEJM).
Lumakras paves the way for direct targeting of oncogenic drivers that were previously inaccessible, illustrating a major shift in therapeutic strategies for lung and potentially other KRAS-mutant cancers.
4. PARP Inhibitor: Rubraca (Rucaparib) Expanded Indication
Rubraca, a PARP inhibitor launched with extended indications in recent years, targets cancers exhibiting homologous recombination deficiency such as ovarian and prostate cancer. By inhibiting PARP enzymes involved in DNA repair, Rubraca induces synthetic lethality in tumor cells with BRCA mutations.
Clinical trials have shown Rubraca's significant efficacy as maintenance therapy post-chemotherapy, improving progression-free survival substantially in ovarian cancer patients. In prostate cancer, Rubraca demonstrated benefit in patients with BRCA or ATM mutations, expanding therapeutic options (Coleman et al., 2017, NEJM; Abida et al., 2020, NEJM).
Rubraca’s expanded indications reinforce the paradigm of exploiting genetic vulnerabilities in cancer and affirm the growing role of PARP inhibitors in personalized oncology treatment regimens.
5. Next-Generation Sequencing (NGS) Liquid Biopsy: Guardant360 CDx
Guardant360 CDx is a comprehensive liquid biopsy test approved by the FDA to detect actionable mutations from circulating tumor DNA (ctDNA) in blood samples. Launched as a non-invasive companion diagnostic, it enables real-time genomic profiling for multiple solid tumors, facilitating tailored cancer therapies without the need for tissue biopsy.
The test covers over 70 genes and reports alterations relevant for targeted therapies, immunotherapy, and clinical trial eligibility. Its rapid turnaround and high concordance with tissue biopsy have made it a preferred choice for patients where tumor access is challenging (Cheng et al., 2020, Clinical Cancer Research).
Guardant360 CDx exemplifies the integration of precision diagnostics into oncology care, empowering clinicians to optimize treatment decisions based on dynamic molecular tumor profiles.
6. Bispecific Antibody: Blincyto (Blinatumomab) Advances
Blincyto, a bispecific T-cell engager antibody targeting CD19 and CD3, has been refined over the last five years with expanded approval for adult patients with B-cell acute lymphoblastic leukemia (ALL). By redirecting T-cells to malignant B-cells, Blincyto evokes potent immune-mediated tumor clearance.
Recent data support its use in minimal residual disease (MRD) positive ALL, demonstrating improved relapse-free survival compared to traditional chemotherapy. Its continuous infusion administration demands rigorous management but is offset by substantial efficacy in hard-to-treat populations (Gökbuget et al., 2018, Lancet Oncology).
Blincyto’s advances highlight the growing impact of immunotherapies that engage endogenous immune cells with precise tumor targeting, offering new hope in hematologic cancers.
7. Personalized mRNA Cancer Vaccines: FixVac (BNT111)
FixVac, developed with mRNA technology, represents a groundbreaking personalized cancer vaccine aimed at treating advanced melanoma. Unlike preventive vaccines, FixVac uses mRNA to stimulate the immune system against tumor-specific antigens, enhancing T-cell responses to eradicate cancer cells.
Early clinical trials indicate an encouraging safety profile and immune activation with signs of tumor regression. The vaccine’s modular mRNA platform allows rapid customization to patient-specific tumor antigens, marking a huge leap in therapeutic cancer vaccination (Kranz et al., 2016, Nature).
FixVac exemplifies the convergence of molecular biology and immunotherapy, offering a novel modality that could extend to multiple cancer types in the near future.
Conclusion
The last five years have ushered in a wave of innovative cancer care products that push the boundaries of treatment efficacy and personalization. From engineered cell therapies and targeted small molecules to advanced diagnostics and novel immune-based approaches, these products illustrate a multi-dimensional approach to combat a complex disease.
As oncology continues to evolve, the integration of precise molecular targeting, patient-specific customization, and non-invasive monitoring will define the next generation of cancer care. These seven products represent significant milestones in this ongoing journey, offering improved options and hope for patients worldwide.
Ongoing research and real-world data will continue to refine these therapies, promising further advancements that translate into long-term survival and better quality of life for those affected by cancer.
References:
Locke et al., NEJM, 2021; Stupp et al., JAMA, 2017; Skoulidis et al., NEJM, 2021; Coleman et al., NEJM, 2017; Abida et al., NEJM, 2020; Cheng et al., Clinical Cancer Research, 2020; Gökbuget et al., Lancet Oncology, 2018; Kranz et al., Nature, 2016.