Featured Articles
- Exploring the Untapped Potential of Gaming Communities in Cancer Support and Awareness
- Harnessing Sound Waves: Exploring Sonic Therapies as an Untapped Aid in Cancer Recovery Programs
- Rediscovering Nature: The Unexplored Healing Power of Indigenous Plants in Cancer Therapy
- The Hidden Role of AI: How Technology is Shaping Cancer Support Networks and Resources
- Top 7 Breakthrough Cancer Care Products Launched in the Last 5 Years: In-Depth Reviews & Rankings
Uncovering the Hidden Role of Gut Microbiome in Cancer Treatment: A New Frontier in Patient Care
Uncovering the Hidden Role of Gut Microbiome in Cancer Treatment: A New Frontier in Patient Care
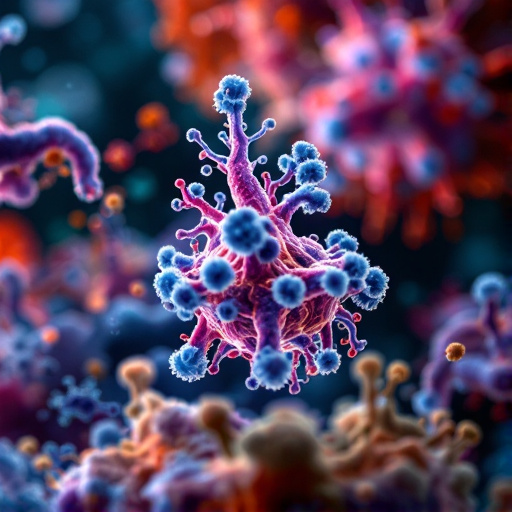
The gut microbiome plays a groundbreaking role in cancer treatment, influencing the effectiveness of therapies and patient outcomes in ways that are only just being uncovered. This burgeoning field of research promises to reshape patient care and open new frontiers in the fight against cancer.
Introduction: The Unseen Warriors
Imagine a bustling metropolis, where trillions of residents collaborate to create harmony or chaos. This vibrant city is your gut microbiome, a thriving community of microorganisms that significantly influence not just digestion, but also your body's response to cancer treatments. The sheer number of microbes here is staggering—approximately 40 trillion! But what if I told you that these tiny entities might hold the key to optimizing cancer therapies?
The Gut-Cancer Connection
Recent studies suggest a potent interaction between gut microbiota and cancer therapy outcomes. The American Association for Cancer Research reported that patients with certain gut microbiome compositions received more benefit from immunotherapy (Zitvogel et al., 2016). In fact, some patients were almost “resistant” to treatments unless their microbiome was in balance. This begs the question: can we manipulate our gut microbiomes to improve cancer treatment results?
What is the Gut Microbiome?
Before diving into its role in cancer, let’s define what we mean by gut microbiome. The gut microbiome comprises trillions of microorganisms living in your digestive tract, including bacteria, viruses, fungi, and even archaea. Collectively, they weigh about 2-4 pounds—roughly the same as the weight of your brain! These tiny entities are vital for digestion, metabolism, and even immune function.
A Journey Through Research
In a groundbreaking study, researchers from the University of North Carolina discovered that patients with a diverse gut microbiome responded better to checkpoint inhibitors—treatments designed to help the immune system recognize and attack cancer cells. This study involved analyzing stool samples to identify the composition of microbiomes in various patients undergoing treatment. They found that those with a more diverse set of microbes had higher response rates, hinting at the body’s intrinsic microbial machinery that influences treatment success.
The Power of Prebiotics and Probiotics
Let’s not skip over the power of nutrition! Diet, supplements, and lifestyle can significantly impact the gut microbiome. Prebiotics—which feed beneficial bacteria—and probiotics, which introduce good bacteria, may enhance the therapeutic effects of classical cancer treatments. For example, a patient named Jane struggled with aggressive breast cancer. After incorporating probiotics into her diet in tandem with her treatment, she reported fewer side effects and an improved quality of life. Interestingly, her oncologist noted her treatment seemed more effective than in similar cases without probiotic usage. Stories like Jane’s are becoming more common, stirring hope for many.
Overcoming the Challenge of Antibiotics
While antibiotics can save lives, they can also dismantle our gut microbe army. Research shows that broad-spectrum antibiotics can reduce microbial diversity, and consequently, treatment efficacy (Vandeputte et al., 2017). This is a double-edged sword—crucial for eliminating infections but potentially detrimental to gut health and cancer treatment. Like a once-bustling city reduced to rubble, a compromised microbiome can lead to complications. The challenge lies in finding a balance and using antibiotics judiciously.
Case Study: Immunotherapy Insights
Consider the case of a 62-year-old man, Mr. Thompson, suffering from advanced melanoma. During his participation in a clinical trial assessing the effectiveness of an innovative immunotherapy, researchers observed a correlation between gut microbiome diversity and treatment outcomes. Mr. Thompson had a relatively diverse microbiome, which—coupled with specific dietary adjustments—dramatically improved his response to the therapy. His experience resonated with both patients and oncologists, leading to discussions on tailored microbiome strategies in cancer care.
Immunotherapy: The Role of Gut Bugs
Immunotherapy is touted as a game-changer in oncology, harnessing the body’s immune system to fight cancer. However, it’s worth noting that not all patients respond equally. Emerging research indicates that the gut microbiome might play a pivotal role in how well patients tolerate and benefit from these treatments. The Journal of Clinical Investigation published findings demonstrating enhanced activation of T-cells—key players in the immune response—when a healthy microbiome was present (Teng et al., 2018). This provides a strong argument for the crucial role of gut flora in modern oncology.
Personalization in Medicine
As cancer treatment evolves, the concept of personalized medicine gains traction. A one-size-fits-all approach may soon be obsolete. By evaluating an individual’s gut microbiome, healthcare providers might customize treatment plans in a manner that maximizes efficacy and minimizes adverse effects. Just think of it as ordering a pizza tailored to your tastes! Instead of the standard pepperoni and cheese, you opt for gluten-free crust and kale, ensuring that every bite nourishes rather than weighs you down.
The Future is Bright: Integrative Health Approaches
As more data pours in, integrative health approaches that encompass gut health and cancer treatments could redefine patient care. From stress reduction techniques and yoga that alleviate anxiety to nutrition plans aimed at enhancing gut health, the future looks promising. Imagine a cancer care plan that doesn't solely depend on chemotherapy but also emphasizes the holistic enrichment of the gut microbiome through diet, lifestyle adjustments, and probiotics!
Cautionary Notes
However, we tread lightly on these captivating revelations. Not all probiotics and prebiotics are created equal; efficacy varies widely among strains and species. Moreover, individual responses can differ dramatically based on existing health conditions, genetics, and lifestyle factors. Therefore, personalized approaches to gut health must be taken thoughtfully, ensuring scientifically backed choices tailored to each patient’s unique microbial landscape.
Conclusion: Embracing a New Paradigm
As we continue to uncover the hidden role of the gut microbiome, it’s clear that it could be a revolutionizing factor in cancer treatment. This new frontier in patient care integrates science with personalized health, providing hope for more effective treatments and improved patient outcomes. As we move forward, the collaboration between oncologists, nutritionists, microbiologists, and patients will serve as a beacon of innovation, leading us into uncharted territories in the fight against cancer.
Are we ready to embrace this exciting journey and unlock the potential of our gut microbiota in our quest for cancer treatment success? The answer, much like everything in life, starts in the gut!
References
1. Zitvogel, L. et al. (2016). "Microbiome and Cancer." American Association for Cancer Research.
2. Vandeputte, D. et al. (2017). "The effect of antibiotics on the human microbiome." Nature Reviews Microbiology.
3. Teng, M. W. L. et al. (2018). "The Role of the Microbiome in Cancer Immunotherapy." Journal of Clinical Investigation.